Diagnostic for Zika virus
Although the Zika virus was first isolated in 1947 in the Zika Forest of Uganda, it was not until the emergence in Brazil in 2015 of this previously obscure tropical disease that it became recognised as a potential pandemic threat. Whilst the symptoms of Zika fever are relatively minor (short term febrile illness combined with a rash, conjunctivitis and arthralgia), it was the dawning realisation of a possible association of the virus with a marked increase in the incidence of fetal neurologic abnormalities which caused alarm. Since 2015, the rapid spread of the Zika virus throughout the tropical and subtropical Americas has led to unprecedented global interest.
The Zika virus itself can only be detected in the bloodstream of patients for a brief period; therefore diagnosis by detection of a class of antibodies (IgM) that appear in the blood soon after infection is more reliable. The problem is that it is hard to tell the difference between antibodies that the body makes in response to the Zika virus from those made in response to its very close relative, Dengue virus. To make matters worse, both viruses are spread by the same species of mosquito so they are equally likely to occur in areas where this mosquito is found. In order to isolate the Zika virus, it is important to be able to distinguish between antibodies that have been raised against a previously encountered virus such as Dengue virus and antibodies that indicate a recent or current virus infection.
In 2016, in response to this global research challenge, the UK Medical Research Council issued a ‘call-to-arms’ under the banner of its Rapid Response Initiative to fast-track research into the Zika virus. As a result, Leaf Expression Systems, in collaboration with the University of Nottingham, received funding of £93,000 to develop a more specific diagnostic test for the Zika virus. Work began on 1 April 2016.
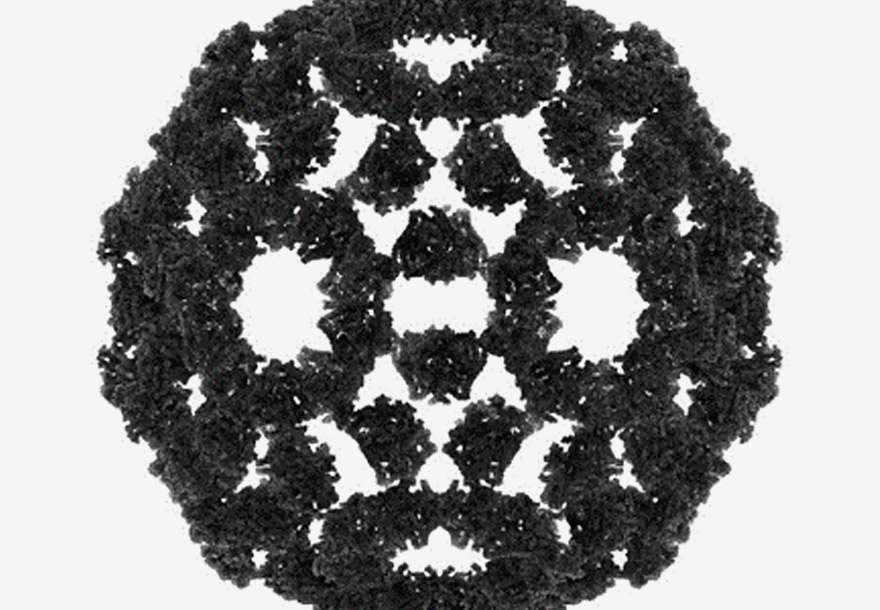
Key to the project is the ability of Leaf Expression Systems’ Hypertrans® expression system to produce the different proteins rapidly. By producing non-pathogenic virus mimics of both the Dengue virus and the Zika virus, the relative antibodies can be detected in parallel. The rapid production of a MAC-ELISA antibody test should result in the highest signal being given against the protein from the virus to which the patient was most recently exposed. Using plant-expressed proteins rather than whole virus, the Hypertrans® system can rapidly introduce specific changes to the proteins so that the test can better distinguish between antibodies that result from the Zika virus infection and those generated by other flaviviruses such as Dengue.
The assays will then be tested using real samples with the assistance of Professor Luis Carlos de Souza Ferreira of the University of Sao Paulo in Brazil.
